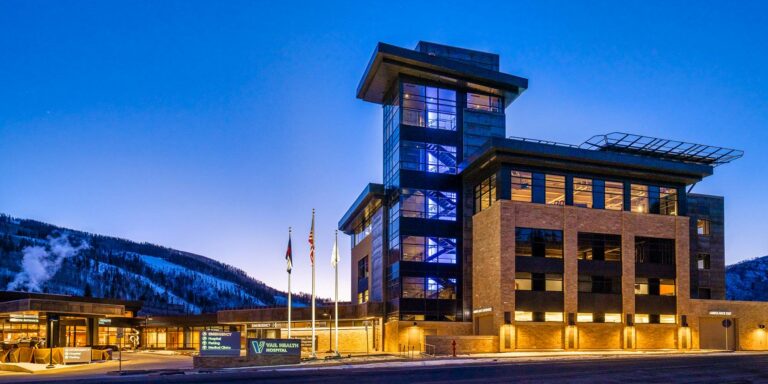
Location
Vail Health Behavioral Health is a non-profit organization based in Vail, Avon, Edwards, and Edwards, providing services across Eagle County. Eagle County is an economically and ethnically diverse county situated in the mountains of central Colorado. The county includes the world-class ski towns of Vail and Beaver Creek, as well as the towns of Minturn, Avon, Edwards, Eagle, Gypsum, Basalt and surrounding areas. The annual population is currently 53,320. However, due to the influx of tourists and second homeowners, the resting population of our community can vary dramatically depending on the season. Eagle County’s population has increased 25% over the last ten years. The local economy is driven by tourism, construction and ranching. The median household income level is $72,214
Organization
The mission of Vail Health Behavioral Health (VHBH; formerly Eagle Valley Behavioral Health) is to lead community collaboration efforts to transform the Eagle Valley’s behavioral health system. VHBH was created to integrate Eagle County’s fragmented and inadequate behavioral health system. VHBH serves as a central hub for integration and coordination of all behavioral health resources, providers, and organizations, which previously operated autonomously lacking in formal or systemic collaborative structure. VHBH strives to eliminate barriers and increase access to behavioral health care targeting all segments of the social, environmental, and healthcare continuum. VHBH acts as the central backbone organization in Eagle County to develop strategic plans for funding, implementing and measuring the impact of behavioral health initiatives, while leading community collaboration to transform our valley’s behavioral health system. Our vision is to imagine a day in Eagle County when we spend as much time, effort and resources on our behavioral health as we do our physical health. In addition to community collaboration and system consultation, VHBH coordinates an internal, psychologically-informed, culturally-responsive Employee Behavioral Health Assistance program (EAP) and provides organizational consultation support for behavioral health organizations and service providers across our community.
Population Served
African American 1%; American Indian 1%; Asian American 1%; Euro-American 40%; Hispanic American 54%; Mid-Eastern American 3%; Gay/Lesbian/Bisexual 15%; . Rural clients: 100%.
The Internship Experience
Interns at VHBH are engaged in a variety of behavioral health services offered through our organization with major areas of focus that strongly align with the areas of focus within COPIC: Behavioral Health Intervention, Community Consultation and Systems Collaboration, Supervision, and Psychological Assessment. VHBH is a leader and coordinator of several behavioral health collaborations, work groups, community-based initiatives, and is viewed as a central hub for the integration and coordination of all behavioral health resources, providers, and organizations within our community. Interns at VHBH have opportunities to engage in behavioral health systems collaboration at state and national systemic level through policy advocacy and leadership development with the Colorado Psychological Association. Interns will provide outpatient therapy through VHBH to the Eagle Valley Community. Additionally, there are three separate tracks available for interns at VHBH: outpatient and assessment (1 FT funded placements), integrated care and outpatient therapy track (1 FT funded placement), and high acuity (1 FT funded placement).
Vail Health Behavioral Health Outpatient Therapy Track (1 intern)
Interns placed with VHBH’s Outpatient Therapy Track support the Vail Health Behavioral Health (VHBH) Outpatient Clinics. VHBH Clinics serve as the community mental health center for Eagle and Summit Counties serving patients from all backgrounds and presenting concerns. As a safety net facility, VHBH has a primary focus on treating patients with depression, anxiety, substance use, and trauma but interns will also get exposure to patients with chronic and persistent mental illnesses.
The intern;s primary clinical responsibilities include brief screenings and longer-term interventions including the provision of individual, family, and couples therapy with children, adolescents, and adults with a variety of presenting concerns. Interns will be responsible for facilitating a number of groups either in the outpatient setting or intensive outpatient program. There will be the opportunity to develop group curriculum based on intern interest or specialty.
Interns may also receive referrals for solution focused, short-term work from the employee assistance program (EAP) for Vail Health employees. In the VHBH Outpatient Clinic, interns will also participate in the psychological testing program completing comprehensive biopsychosocial assessments and conducting neuropsychological batteries.
The Outpatient Therapy Track also offers the unique opportunity to be involved in leadership roles in many Community Consultation Systems including but not limited to: Zero Suicide Committee, Rural Communities Opioid Response Program, Eagle County Crisis Response Debrief, Disaster Behavioral Response Committee, Critical Incident Debrief Team, and more. The Outpatient Therapy also services the Latinx Community of Eagle County offering multiple opportunities for community engagement, bilingual service delivery, and program development.
Vail Health Behavioral Health Integrated Care & Outpatient Therapy Track (1 intern)
Interns placed with VHBH’s Integrated Care & Outpatient Therapy Track support the Integrated Behavioral Health program at Colorado Mountain Medical (CMM) and Vail Health Behavioral Health (VHBH) Outpatient Clinic. In the Integrated Care rotation, interns are embedded into the medical clinic supporting patients accessing primary care, dermatology, gynecology, endocrinology, urology, and pediatrics. Interns will field warm hand-offs from physicians, consult with medical staff, and provide brief, solution-focused interventions to patients, their parents, and families. Interns will also have the opportunity to attend physician meetings, build presentations for staff on treating behavioral health patients, and participate in the development of a specialty project related to primary care.
While rotating through VHBH Outpatient Clinic, interns primary clinical responsibilities include brief screenings and intervention including the provision of individual, family, couples, and group therapy with children, adolescents, and adults with a variety of presenting concerns. Interns may also receive referrals for solution focused, short-term work from the employee assistance program (EAP) for Vail Health employees. In the VHBH Outpatient Clinic, interns will also participate in the psychological testing program completing comprehensive biopsychosocial assessments and conducting neuropsychological batteries.
Vail Health Behavioral Health High Acuity Track (1 intern) *Formerly the Your Hope Center Crisis Track
In partnership with Your Hope Center, the Vail Health Behavioral Health High Acuity Track offers an immersive experience for interns dedicated to serving individuals with acute behavioral health concerns. This track has evolved from the original Your Hope Center Crisis Response Track to provide a broader scope of care. Interns in this track will spend two days a week in VHBH outpatient clinical services, providing individual, family, couple, and group psychotherapy for patients experiencing high-acuity behavioral health challenges. This will include participation in VHBH High Intensity Services Program. This program includes the VHBH Intensive Outpatient Program which offers 6 hours of group, weekly to adolescents, and 9 hours of group, weekly to adults. It also includes community-based stabilization for patients that do not require hospitalization. Interns will support in curriculum development, facilitation of group, and administrative support as well as safety planning, motivational interviewing, cognitive behavioral therapy (CBT), and communication skills training. Evening and weekend hours may be necessary to support the High Intensity Services programming.
In addition to high acuity outpatient, the interns will have the opportunity to rotate through additional high acuity service lines:
- Your Hope Center Crisis Co-Mobile Response: Working alongside law enforcement and paramedics to conduct risk assessments, facilitate de-escalation, and connect individuals to necessary resources. Weekend and evening hours may be required.
- Precourt Health Center: 28 bed inpatient psychiatric facility for acute behavioral health needs. Interns can perform individual, family, couples’ sessions in the unit as well provide milieu and group interventions. Weekend and evening hours may be required.
Elective Focus Areas
Elective training tracks are selected by the intern and can be selected for the year or on a semester basis for both tracks. Possible elective areas of focus include:
- Suicide prevention, mental health first aid, and community engagement
- Wellness, vicarious-trauma, and burn out prevention
- Early Childhood parenting classes, parent engagement, and psychological assessment
- Psychological Assessment (both adult and children available)
- Community Outreach/Latinx Community Outreach
- Integrated Primary Care (CMM only)
- LGBTQ+ Community Engagement
- Research/Grant Writing/Development
- Orthopedic Surgery: Observation of orthopedic surgeries (Howard Head only)
- Alpine Skiing Events: Interns who are capable of skiing may provide consultation during alpine skiing events (Howard Head only)
- Pain Management
Training Philosophy
Our training philosophy follows 6 core principles that serve as the foundation for the training, learning environment, and professional development. The points below outline our aspirations for our training program, our expectations for the treatment of others, and our expectations about personal behavior as an EVBH employee.
A wide-scope training and solid generalist practice is pertinent for developing the needed foundation to become an advanced professionalDiverse and interrelated knowledge and skills are essential for effective and comprehensive practice/care. We value knowledge contributions from our own disciplines and from other related professional disciplines.
Learning is optimized in an environment that is supported, developmentally graduated, and challenging.
We want trainees and staff to feel that their opinions, knowledge and skills are valued, and that it is safe to make mistakes. It is also essential for growth that trainees can honestly evaluate their strengths and limitations. In this way, growth areas and blind spots can be addressed and feedback can be integrated.
Sound psychological theory and research are the underpinnings of effective practice.
Interventions and practice must be guided by both theory and practice. Staying current on scientific research and evidence based practice helps ensure more effective interventions and case conceptualizations that drive treatment. Using research to guide practice also ensures a high level of ethical professionalism
All staff members are expected to demonstrate a commitment to self-awareness and an understanding of the intersection of the personal and professional.
To be a good mental health professional, skill acquisition is tantamount. What is more important is self understanding, personal maturity, self regulation, and ethical behavior. We expect staff to continually self-reflect about performance, professionalism, and growth. Leadership is also dedicated to helping staff reflect and make changes along this continuum.
Each staff member has the right to be treated with respect.
All staff members deserve to have a voice and to be intrinsically valued. Honest communication and cooperation among staff are essential to meet larger goals. Each staff member is charged with creating a supportive environment for their colleagues so that individuals have an equal opportunity to do their work, realize their goals, and feel comfortable.
Respect for diversity is the common core for all activities
We expect all staff and trainees to commit to learning about equality, inclusion, power/privilege, implicit bias and diversity. All staff will demonstrate a willingness to examine their own assumptions, behaviors, and values so that they may work effectively with cultural, individual, and role differences, including those based on age, gender, gender identity, race, ethnicity, culture, national origin, religion, sexual orientation, disability
Faculty Information

Y. Evie Garcia, Ph.D., LP
Primary Supervisor
Dr. Evie Garcia earned a BA in Psychology, a Master’s in Counseling and a PhD in Counseling Psychology from Arizona State University, including a year-long internship in neuropsychology at the Palo Alto VA Medical Center in Palo Alto, CA. She completed a two-year postdoctoral fellowship in neurorehabilitation at Gentiva Rehab Without Walls in Phoenix, AZ. Dr. Garcia has been training counselors and psychologists for more than 25 years. She came to Vail Health Behavioral Health from Northern Arizona University in Flagstaff, AZ where she was a tenured Professor and served as the Doctoral Training Director for the PhD program in Counseling Psychology and School Psychology for nine years, as well as Associate Dean of the Graduate College for six years. Dr. Garcia has numerous publications, conference presentations, and grants related to diversity and health. She served as President of several national associations, including the Council of Counseling Psychology Training Programs, APA Division 45 – Society for the Psychological Study of Culture, Ethnicity, and Race, the National Latinx Psychological Association, and the Arizona Psychological Association. She was awarded the 2023 Aaron and Matty Canter Award for Lifetime Achievement in Psychology and the 2022 Award for Distinguished Contributions to Science from the Arizona Psychological Association.
Email: Yolanda.Garcia@vailhealth.org
 Paige Baker-Braxton, Psy.D., LP
Paige Baker-Braxton, Psy.D., LP
CO-PIC Training Director & Secondary Site Supervisor
Dr. Paige Baker-Braxton (she/her) attended Georgetown University receiving undergraduate degrees in Psychology and Gender Studies. She pursued both a MS and doctorate in multicultural Clinical Psychology from Nova Southeastern University. Dr. Baker-Braxton trained as a Psychology Fellow in 1 of 10 national sites specializing in LGBT Mental Health in the VA. Dr. Baker-Braxton spent much of her career working in primary care behavioral health settings and working with queer and transgender survivors of sexual and intimate partner violence. In 2021, she was hired by Vail Health as Director of Outpatient Behavioral Health. In this role, Dr. Baker-Braxton oversees all outpatient and intensive outpatient therapeutic services, supervises the behavioral health training programs, and runs the Integrated Behavioral Health department.
Email: paige.braxton@vailhealth.org
Contact Information
Site Director: Y. Evie Garcia, Ph.D., LP
Email address: Yolanda.Garcia@vailhealth.org
Phone: (970) 445-2489
Website: www.vailhealthbh.org
Mailing address: PO Box 1529 Vail, CO 81658

